Scientists have made a groundbreaking discovery by uncovering brain signals that indicate the level of pain experienced by individuals. This significant finding offers hope for innovative treatments targeting chronic pain that severely impacts people’s lives.
For the first time, researchers have deciphered the brain activity associated with chronic pain in patients. This development raises the possibility that brain stimulation therapies, already effective in treating Parkinson’s disease and major depression, could provide much-needed relief for those who have exhausted other options.
The research team, led by Prasad Shirvalkar, a neurologist at the University of California, San Francisco, found that chronic pain can be accurately tracked and predicted in real-world scenarios. This means that pain levels can be assessed while patients engage in everyday activities such as walking the dog, at home, or during morning routines, providing valuable insights into their pain experiences.
Chronic pain, often referred to as a “silent epidemic,” affects nearly 28 million adults in the UK alone, representing approximately 44% of the population. Despite medication and treatment, individuals endure persistent pain for at least three months. The causes of chronic pain are diverse, encompassing conditions such as arthritis, cancer, back problems, diabetes, stroke, and endometriosis.
Despite the escalating use of potent opioids to manage chronic pain, existing medical treatments yield limited effectiveness. Consequently, experts are calling for a comprehensive reassessment of how healthcare services approach patients suffering from long-lasting pain, in light of these challenges.
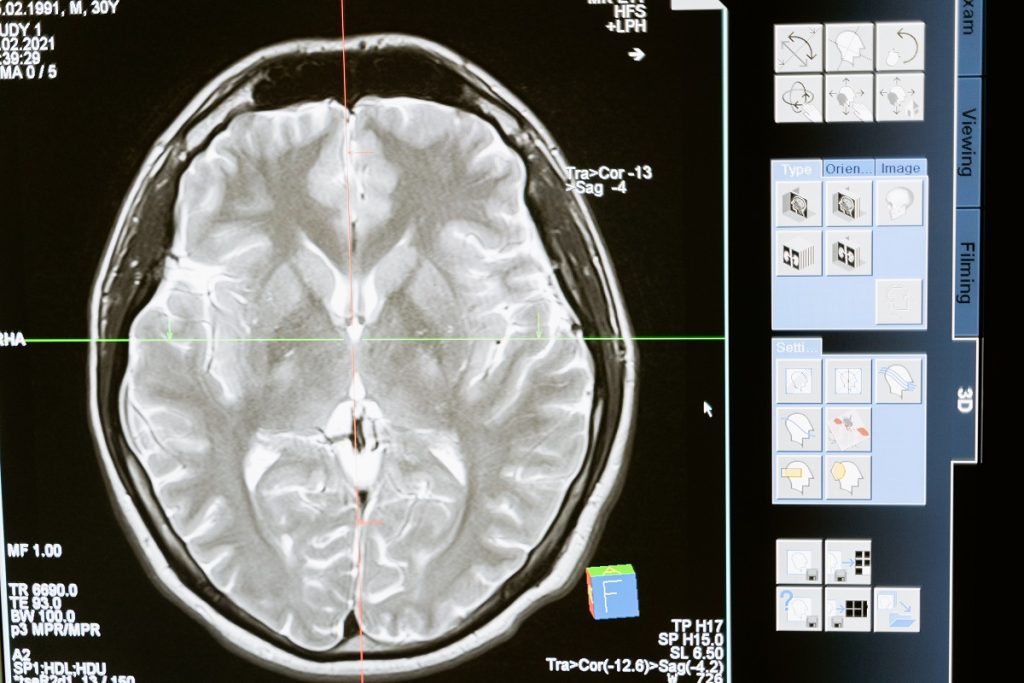
In a recent study published in Nature Neuroscience, Shirvalkar, and his colleagues conducted surgical procedures to implant electrodes in four patients suffering from intractable chronic pain following a stroke or limb loss. These implanted devices enabled the patients to capture brain activity in two specific regions: the anterior cingulate cortex (ACC) and orbitofrontal cortex (OFC) by simply pressing a button on a remote control.
Throughout the day, the volunteers were asked to complete brief surveys regarding the intensity and nature of their pain, while also recording snapshots of their brain activity. By combining the survey responses with the recorded brain data, the researchers successfully trained an algorithm to predict an individual’s level of pain based on the electrical signals detected in their OFC. Shirvalkar described this achievement as the development of an “objective biomarker” for this type of pain.
Additionally, the team’s separate investigations revealed distinct brain activity patterns associated with acute or short-term pain, such as the pain experienced when touching a hot object to the skin. These findings shed light on why routine painkillers are often less effective for chronic pain compared to the intense but momentary pain resulting from a stubbed toe.
Shirvalkar emphasized that chronic pain is not merely a prolonged version of acute pain; it exhibits fundamental differences in the brain. The hope is that by gaining a deeper understanding of these distinctions, the obtained information can be utilized to develop personalized brain stimulation therapies for the most severe forms of pain.
These findings have the potential to significantly impact ongoing clinical trials exploring deep brain stimulation (DBS) as a means to manage chronic pain. DBS involves delivering electrical pulses to the brain to disrupt problematic signals. While it is considered a treatment option of last resort due to the required brain surgery, DBS is already used for conditions such as Parkinson’s disease and major depressive disorder. For effective implementation, precise identification of the targeted signals is crucial.
Professor Blair Smith, an expert in chronic pain at the University of Dundee who was not involved in the research, highlighted the challenges faced by doctors in assessing the effectiveness of treatments due to the lack of objective pain measures. He expressed optimism about the potential extension of this research, as it not only offers the opportunity to objectively measure certain types of pain but also enhances our understanding of the underlying biological mechanisms.
However, Smith cautioned that pain is a complex phenomenon influenced by psychological, social, and cultural factors, as well as previous pain experiences and expectations. He invoked Nassim Taleb’s analogy of studying ink to understand literature, emphasizing the intricate nature of pain and the need to consider multiple factors when examining it.
Based on my knowledge update in September 2021, there haven’t been any specific breakthroughs in which scientists have discovered brain signals specifically related to chronic diseases. However, it is important to acknowledge that research in neuroscience and medicine is continually progressing, and there may have been advancements since then.
Brain signals, such as those measured through electroencephalography (EEG) or functional magnetic resonance imaging (fMRI), are crucial for understanding brain function and can provide insights into various neurological conditions. Extensive studies have been conducted on these signals in relation to conditions like epilepsy, Parkinson’s disease, Alzheimer’s disease, and mental health disorders.
Chronic diseases typically encompass enduring conditions like diabetes, cardiovascular disease, autoimmune disorders, or certain types of cancer. While the brain is involved in regulating various bodily functions, the specific brain signals associated with chronic diseases may not be well-defined or fully comprehended.
Nonetheless, ongoing research aims to explore the connections between the brain and chronic diseases. Advances in neuroimaging techniques, machine learning, and data analysis may aid in identifying patterns and potential biomarkers associated with chronic conditions. This could contribute to a better understanding of the underlying mechanisms and potentially lead to new diagnostic or therapeutic approaches.